Mini brains have been grown in the lab out of cells taken from dementia and motor neurone patients, opening the door for new treatments.
Being able to grow small organ-like models of the brain allowed researchers from the University of Cambridge to understand what happens at the earliest stages of a form of motor neurone disease known as amyotrophic lateral sclerosis.
This condition often overlaps with dementia and tends to occur in younger adults aged 40-45.
The mini brains help scientists see how the condition develops long before any symptoms begin to emerge, and in turn screen for potential drugs.
These conditions cause devastating symptoms of muscle weakness with changes in memory, behaviour and personality, that can be eased if caught early enough.
In the future, the researchers hope individual mini brains could be created from a person's skin cells and used to develop and test personalised drugs to treat their specific symptoms.

Mini brains have been grown in the lab out of cells taken from dementia and motor neurone patients, opening the door for new treatments, according to researchers
One medication tested on the artificial brains was found to destroy toxic proteins that gather in clumps, say Cambridge University scientists.
Study leader Dr Andras Lakatos said: 'Neurodegenerative diseases are very complex disorders that can affect many different cell types and how these cells interact at different times as the diseases progresses.
'To come close to capturing this complexity, we need models that are more long-lived and replicate the composition of those human brain cell populations in which disturbances typically occur, and this is what our approach offers.
'Not only can we see what may happen early on in the disease - long before a patient might experience any symptoms - but we can also begin to see how the disturbances change over time in each cell.'
The models were cultivated for almost a year, enabling analysis of dementia-related disorders over a long period.
They were derived from patients with FTD (frontotemporal dementia) and ALS (amyotrophic lateral sclerosis) - a common form of motor neurone disease.
The conditions cause muscle weakness and memory, behaviour and personality problems - and can affect people in their 30s and 40s.
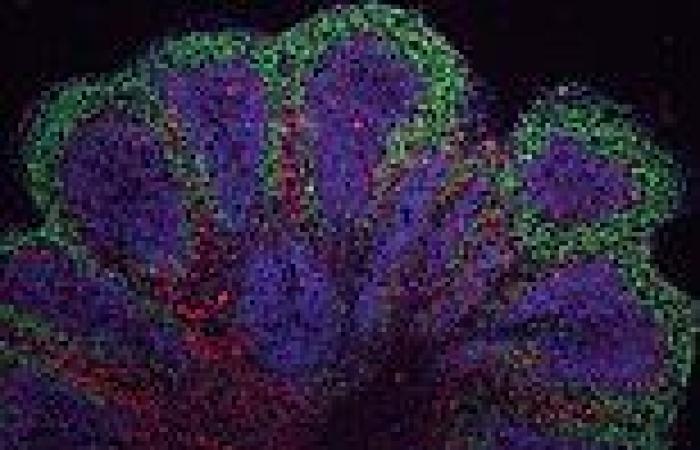
The mini brains, or 'organoids', show what happens long before symptoms emerge, and can screen potential therapies.
Brain tissue previously created in the lab has only lasted a short time, limiting the scope for experiments, but this experiment survived for 340 days.
During that time it harboured the most common genetic mutation in FTD and ALS.
Instead of balls of cells, the 3D cultures were cut into slices, ensuring they received the necessary fuel.
'When the cells are clustered in larger spheres, those cells at